The policy void surrounding prisoners who lose their mental capacity behind bars
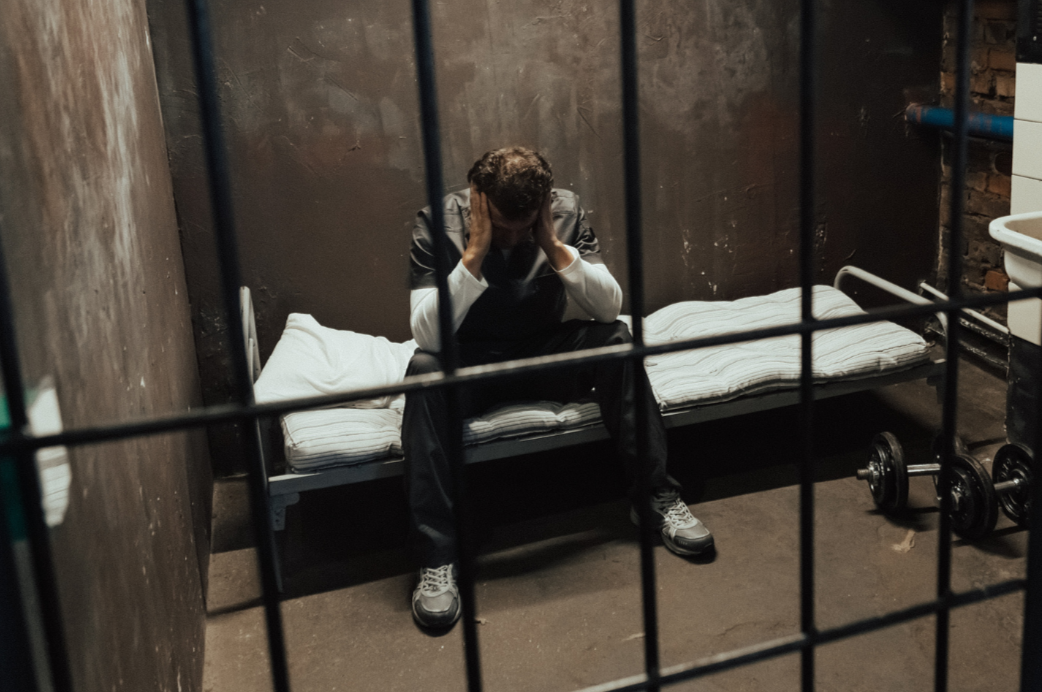
It’s not a particularly controversial fact that most people who enter the prison system already experience some form of psychological, physiological, or emotional dysregulation. Traumatic backgrounds, adverse childhood experiences, low literacy levels, language barriers, and a wide range of mis-managed or undiagnosed mental and physical health needs make up a significant proportion of the prisoner population.
Once individuals enter the prison system, their existing needs are often exacerbated by deteriorating and outdated facilities, a lack of mental health resources, restricted routines and communication, minimal stimulation, and a constant state of fight-or-flight due to the very nature of the environment—alongside the many other painful realities that accompany serving a prison sentence.
“An emerging trend within this landscape is the increasing number of individuals who begin to experience significant mental health decline during their sentence, and the ways in which this is (or isn’t) transparently recognised and addressed.”
The prison population is both increasing and changing within an infrastructure that was never designed—and no longer has the capacity—to address the problems it now faces, many of which are of its own making. People are serving far longer sentences, and many are ageing or becoming debilitated behind bars. An emerging trend within this landscape is the increasing number of individuals who begin to experience significant mental health decline during their sentence, and the ways in which this is (or isn’t) transparently recognised and addressed.
While Samaritan helpline posters may be visible and wing application forms to see the GP accessible, there is a lack of clear policy outlining what happens when a person loses capacity within the prison system. How is a decline recognised, especially if it unfolds quietly? Who needs to be informed, and who holds responsibility for assessing the needs of someone who is significantly deteriorating or has deteriorated? Who makes decisions in the person’s best interests, and what happens when the individual is unable to advocate for themselves or engage due to withdrawal, lack of insight into their mental state, or dissociation? How is this followed up between prison transfers, given that medical files are rarely readily available when a prisoner is newly admitted to a different facility? Ultimately, who is responsible for ensuring that a person with severe medical and mental health needs receives appropriate care while living on a prison wing?
A common underlying theme in these cases is the reluctance of prisoners to seek help when they first detect their mental health deteriorating, as they fear that disclosing their struggles will be used against them. Within the system, being perceived as “unstable” often results in increased scrutiny, tighter restrictions, or further criminalisation, rather than meaningful support.
For those who have no one on the outside—or anyone inside—able to advocate for them, prisoners are often left to deteriorate alone. At best, they may receive limited help from a fellow prisoner or a compassionate staff member, but too often, that is where their luck runs out. For those experiencing severe mental health conditions and deterioration, they can become effectively buried alive within a system that lacks the policy guidance, infrastructure, and resources to notice or address their needs. For those prisoners who do have someone on the outside, the legal and emotional burdens often fall on their loved ones, who can only watch the decline from afar—calling for help through limited channels of communication in a tiring, relentless struggle.
“When contact is lost due to mental health decline, these individuals become “ghosts in the system.” It becomes much harder to regain or sustain contact once they have completely slipped from a loved one’s grasp.”
As prisoners’ mental health declines, many disengage from the prison system and its services—not by choice, but because their deterioration leaves them unable to navigate its protocols. Through prolonged periods of imprisonment, continuous untreated or mis-managed mental ill health, and communication barriers, many prisoners become estranged from their loved ones, leaving families unable to communicate concerns effectively to the holding establishment as the person dissipates into the depths of the prison system. When contact is lost due to mental health decline, these individuals become “ghosts in the system.” It becomes much harder to regain or sustain contact once they have completely slipped from a loved one’s grasp.
Peeling back the layers further, the deeper issue is that prisoners—and people in general—with serious mental health conditions often do not recognise that they are unwell. As a result, the prison system tends to fall back on its default assumption: that those who disengage or fail to respond to concerns are doing so by choice, because they are presumed to be cognitively responsive. Too often, the system refuses to acknowledge that a prisoner may have deteriorated to the point where they can no longer effectively advocate for themselves. For loved ones, navigating the resulting legal and bureaucratic barriers becomes an exhausting battle.
When families or advocates raise concerns, prison services and organisations often insist that appropriate safeguards are in place—citing access to services and existing procedures such as complaints processes or medical applications. However, if the prisoner lacks capacity or does not recognise their own mental health needs, this can create a negative feedback loop, leaving them increasingly neglected within the system while their loved ones are left helpless and limited in how much they can intervene.
If a prisoner has not given consent for an appropriate person to engage on their behalf—whether due to mental impairment, distrust of internal authorities, or having completely fallen through the cracks—the situation becomes “a very grey area,”. This is why, in such circumstances, people rely on prison staff and medical professionals to take the right initiative, and to record and respond to loved ones’ concerns submitted through the family communication gateway system, ensuring the prisoner’s best interests are recognised and acted upon.
In reality, however, the high turnover of staff and the limited time that professionals working in prisons can spend with prisoners mean that even brief direct contact is minimal. Without consistent interaction, it can be difficult to determine whether a prisoner is mentally unwell—particularly for those whose mental health difficulties are not outwardly apparent, and when there is no clear benchmark against which to assess their current state.
Figure 1. A Cycle of Inaction, where a prisoner’s mental health deteriorates.
A Cycle of Inaction (see Figure 1)
1. Mental Health Deteriorates
Gradual loss of contact with both the inside and outside world
2. Concerns Raised
Families, fellow prisoners, or staff notice the decline
Concerns are reported to prison and health authorities on the prisoner’s behalf
3. Lack of Engagement from the Prisoner
The individual does not recognise their own mental health issues
They may refuse help or fail to engage with support services
4. Advocates and Referrals
Advocates make referrals to agencies or mental health services to escalate concerns
Agencies face policy and data protection constraints
5. Requirement for Prisoner Consent
Agencies need the prisoner’s consent to act (without consent, little or no intervention can take place)
6. The Catch-22
If the prisoner withholds consent, the process stalls
If the prisoner grants consent, they may be deemed “mentally capable” and therefore responsible for managing their own affairs
The prisoner may pretend to be okay for fear of further scrutiny
7. The Endless Loop
Loved ones and advocates continue to raise concerns
The cycle of reaching dead ends continues, with the prisoner’s condition worsening
So, how is this resolved? There is no clear pathway or accessible official policy. The prisoner is left at the mercy of the system, while families must tirelessly advocate to show that the individual has disengaged due to mental health decline and can no longer make decisions in their own best interests—hoping the system will listen and take the right action. This raises a critical question: how can legal action be pursued when the prisoner in question is seemingly mentally incoherent and will not provide consent for those who have their best interests to act on their behalf?
“prisons are rapidly becoming de facto mental health asylums, absorbing the spill-over of individuals who really need psychiatric or medical care.”
One option is the Court of Protection route—a long and winding process, but one worth pursuing if someone’s life is at risk. Prevention is better than cure. Unfortunately, it is now recommended that prisoners, while they still have capacity and are serving a relatively long sentence—or if mental or medical health issues are foreseeable—consider granting a Power of Attorney to someone they trust to act in their best interests.
There is no clear-cut solution, but CJS professionals, legal experts, and families of prisoners, agree that this remains a very grey and neglected area of policy within the prison health care system. Unfortunately, it is a gap that will only become more apparent as the system faces increasing strain and disorder, fewer experienced staff to monitor and address concerns, growing complex mental health needs, limited resources, increasingly strict data protection rules framed as safeguarding and security measures, and a growing population of prisoners serving very long sentences.
With more prison placements being created, limited resource investment, and a shortage of mental health beds, prisons are rapidly becoming de facto mental health asylums, absorbing the spill-over of individuals who really need psychiatric or medical care. The absence of safety-nets around this issue raises serious safeguarding concerns, including questions about preventable self-harm, violence, and deaths. Unless prisoners are treated as people in need of care—not merely as “offenders”—these cycles of institutional failure, systemic disregard and invisibility will continue.
Scroll down to join the discussion
Disclaimer: This article is for information purposes only and is not a substitute for therapy, legal advice, or other professional opinion. Never disregard such advice because of this article or anything else you have read from the Centre for Male Psychology. The views expressed here do not necessarily reflect those of, or are endorsed by, The Centre for Male Psychology, and we cannot be held responsible for these views. Read our full disclaimer here.
Like our articles?
Click here to subscribe to our FREE newsletter and be first
to hear about news, events, and publications.
Have you got something to say?
Check out our submissions page to find out how to write for us.
.