UK government’s Men’s Health Strategy – submission by the Centre for Male Psychology
In July 2025 the UK government’s Department of Health and Social Care had a call for submissions of information about men’s physical and mental health in England. It was open to organisations, academics and individuals, and called for evidence on three main areas:
1/ The factors driving behaviours posing a risk to health among men and boys,
2/ Suggestions for improving health outcomes for men and boys, such as on mental health and suicide prevention, and
3/ Improving men’s access, engagement and experience of the health service.
Here is the submission from the Centre for Male Psychology, followed by a few concluding comments on the overall review process:
1/ Factors driving behaviours posing a risk to health among men and boys
The answers here will focus on men’s mental health and suicide. The answers are not intended to be exhaustive; this is a complex field and no doubt other submissions will raise valid and useful points too. Note that where I mention sex differences in behaviour, I am referring to men and women on a population level, not an individual level.
Several factors drive behaviours that put men’s mental health at risk. I will focus in this section on health literacy, expression of symptoms, life events, and sex differences in the experience of stressful events.
Lack of health literacy leading to less help-seeking
Many men don’t realise when they are experiencing mental health problems. This is often misattributed to men lacking the ability to mentalize / introspect, but there is a much more likely explanation, related to symptom expression, which I will describe in the following section.
Symptoms of male-typical depression and trauma
Most people don’t recognise male-typical depression. By ‘most people’ I mean both men themselves and the health professionals who should be helping them. Many men experience depression and trauma differently than women do. For example, whereas women tend to cry and want to talk to others about their problems, men tend to become angry or aggressive, and may turn to substance abuse as a form of self-medication. Other symptoms may include working long hours, playing video games for extended periods, gambling. Although substance abuse is sometimes recognised as self-medication, often it is seen as an issue in its own right.
Because male depression is so little recognised even by mental health professionals, there has been almost no effort to raise public awareness through health promotion campaigns. An exception to this was the ‘A CLAM’ campaign by The Centre for Male Psychology in 2023, but this had no support from the NHS or other large platforms, so had limited reach. The key point is that if nobody tells men what symptoms to look out for, they have less chance to realise they are depressed. Similarly, if their family and friends don’t know what male-typical depression looks like, they can’t recognise it in someone else, so don’t know how to deal with it. Although this sex difference in expression of symptoms is beginning to be recognised in some parts of academia and clinical psychology, it is not yet widely enough recognised to be part of the health literacy of young men e.g. through health promotion campaigns.
Stressful life events
It is important to realise that mental health problems are often the result of external forces, such as relationship breakdown, and adverse childhood events (ACEs). These events can cause male-typical depression behaviours, such as aggression and substance abuse. Thus anything that causes stress can lead to problem behaviours.
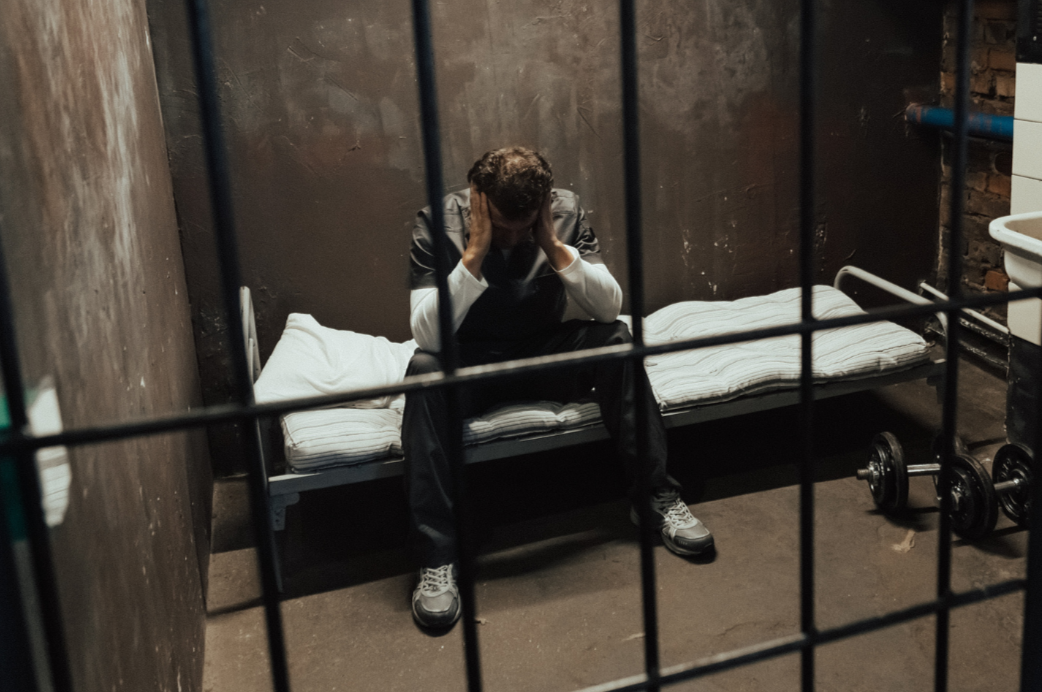
Precursors of suicide
Let’s focus here on the precursors of suicide, which are fairly well established. Primarily this is relationship problems, accounting for 40% of suicides. Men can suffer extreme stress due to losing child custody and having a negative experience in the family courts. The second most common reason for suicide is work/money problems, accounting for 22% of suicides and being accused of wrongdoing or crime (9%), which may be relevant to the men who suffer extreme stress due to being falsely accused of sexual abuse. Other precursors include long-term health problems which are associated with 28% of suicides, though are not necessarily a direct cause of suicide. Masculinity: Pirkis et al (2017) found the main predictors of suicidality are – in descending order of magnitude – depression, life events, alcohol abuse, being single, and – with important caveats described below - masculinity. The issue of masculinity and mental health is complex and generally misunderstood in significant ways, and is a topic I expand on in the later sections on improving health outcomes and improving health interventions.
Sex difference in experience of stressful events
Stressful life events can cause depression in women too, but the important issue is that the results may be different for each sex for various reasons: (a) differential expression of symptoms; (b) the way events are experienced differently by men and women e.g. men get treated more harshly in the family court system, so have a greater burden of stress from family court experiences; (c) women are more likely to seek help and be offered help; and (d) the help available (talking about feelings) is more suited to women than men. This problem is compounded by men being urged to talk about their problems, or how they feel about their problems, but often finding that people really can’t relate to their problems. This latter issue might relate to the fact that around 80% of therapists are women, who might therefore find it hard to understand issues from a male perspective e.g. find it hard to believe that men can be victim of domestic violence by a woman, or that men suffer more than women through family breakdown. They might also see men as being difficult clients e.g. wanting practical solutions rather than wanting to talk about feelings.
2/ Suggestions for improving health outcomes for men and boys, such as on mental health and suicide prevention
Firstly, address the life events that impact mental health, not just mental health. For example, before a man is suicidal because of child custody, there are key time points at which support may be vital. For example, during the family court process, offer him legal support and mental health support, which is especially important if he feels he is dealing with false allegations of abuse. Organisations like Both Parents Matter are already trained to appropriately offer these kinds of support. Preferably the intervention should be preventative: long before the relationship has broken down to the point it is being dealt with by the family courts, couples should be offered couples counselling, and it’s important that such counselling should not routinely take the side of the female partner, as is anecdotally so often the case. After the family court ruling, a man with reduced or no access to his family and with a lapsed friendship group very much needs help to counter the social isolation that so often is experienced by divorced dads.
As a side issue, there is an good argument that suicide should not be treated as a mental health issue, because although it can be argued that nobody in their right mind would take their own life, the reality is that many if not most male suicides are caused by stressful life events, such as family court issues. Improving outcomes related to men’s mental health, including reducing suicide, means addressing the social factors that influence these outcomes e.g. family courts, false allegations with no consequences for the accuser, workplace stress etc.
When mental health services come into play, it is essential that the therapist is trained to understand men’s experiences and be able to empathise with men. Empathy is the key factor in the success of therapy, but unfortunately many therapists are trained to see men’s problems as caused by patriarchy, privilege or masculinity, all of which obscure the lived experiences of men and are thoroughly non-empathic viewpoints. In general, a ‘deficit model’ of masculinity is taught to trainees, which does not equip therapists do approach men’s problems in a realistic way. It is important to note that men thinking masculinity makes them behave badly (e.g. feel violent towards women, or bottle up their feelings) is correlated with worse mental wellbeing, so this type of thinking should be avoided by therapists (Barry, 2023).
To what extent are services in these areas are currently meeting the needs of men?
It has to be said that men are significantly let down, and the cost in terms of mental health is inestimable.
Suggestions as to how services for health conditions that affect men can be improved to better meet their needs
First, it needs to be understood that men experience different stressors to women (e.g. family court, false allegations of abuse), express symptoms of distress differently, and have different needs in terms of therapy. At present there is almost no training on meeting men’s mental health needs, and where men’s mental health is addressed, it is often based on the deficit model, which is unlikely to help men. Diluted versions of the deficit model (e.g. ones which blame ‘gender norms’ for men’s problems) are also inadequate in terms of genuine empathy and are unlikely to help. The need to address this issue is urgent and long overdue.
A related issue is that around 80% of therapists are women. Many of them do a fantastic job, but being a woman probably doesn’t help them in terms of relating to men on a deep level. That is not to say that male clients should only be treated by men (although some men will prefer a male therapist, especially if their problem is related to women e.g. being a male victim of domestic violence), and indeed it’s not to say that all male therapists are better at working with male clients. The training of the therapist is more important than their sex. It should be noted too that training courses are predominantly female, typically are influenced by the deficit model of masculinity, and may be experienced as hostile environments for heterosexual male trainees.
Identify gaps in data or evidence on these areas
Part of the problem of gamma bias is that these issues have been largely overlooked, resulting in a dearth of data and evidence on these important issues. More research is urgently needed to create an evidence base for therapy that works for men. The Centre for Male Psychology is happy to undertake this work.
3/ Improving men’s access, engagement and experience of the health service
The answers here will focus on men’s mental health and suicide.
Examples of solutions that have improved men’s engagement and experience of healthcare services
Men’s Sheds. These are spaces where men can meet to engage in activities such as fixing garden furniture. There is no pressure to talk about feelings or engage in therapy in any way. Nonetheless there is evidence that Men’s Sheds improve men’s wellbeing and reduce social isolation.
Sports and activities. Men in general are more inclined to seek solution-focused interventions (e.g. discussing how to fix their problem) rather than interventions that require them to talk about their feelings. Also men tend to like action-orientated activities such as weight training more than women do. Some psychologists have found that adding a sports and exercise aspect to interventions for men’s mental health has the potential to increase socialisation and improve mental health.
Listening to men. The mental health support line Samaritans found that male callers stay on the line for less time than female callers, and ring off more often. However after a series of workshops (described in Seager, 2019) for the helpline workers, aimed at helping them understand men better, male callers subsequently stayed on the line for significantly longer than they had previously.
Recommendations for how healthcare services can improve how they engage men and the experience they offer
As well as the above examples, here are four key sources of information on how specifically to improve therapy for men:
Liddon, L., Kingerlee, R., Seager, M., Barry, J.A. (2019). What Are the Factors That Make a Male-Friendly Therapy? In: Barry, J.A., Kingerlee, R., Seager, M., Sullivan, L. (eds) The Palgrave Handbook of Male Psychology and Mental Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-04384-1_32
Chapter 11: Mental health, therapy, and support strategies, in Liddon, L., & Barry, J. (2021). Perspectives in male psychology: An introduction. John Wiley & Sons. ISBN: 978-1-119-68535-7
Seager, M., & Barry, J. (2022). Psychological interventions to help male adults. The British Psychological Society. https://discovery.ucl.ac.uk/id/eprint/10170520/1/Barry_Practice%20Briefing%20-%20psychological%20interventions%20to%20help%20male%20adults%2019-11-22.pdf
Liddon, L., Kingerlee, R., & Barry, J. A. (2018). Gender differences in preferences for psychological treatment, coping strategies, and triggers to help‐seeking. British Journal of Clinical Psychology, 57(1), 42-58 https://bpspsychub.onlinelibrary.wiley.com/doi/abs/10.1111/bjc.12147
I will add to this a few points which should be emphasised: Empathy is the key factor in the success of therapy. Much of the training of therapists today encourages trainees to focus away from men’s perceptions of their problems and instead focus on their place within theoretical structures (e.g. hegemonic masculinity, patriarchy theory) as a way to explain why men have problems. Interventions (e.g. to reduce intimate partner violence) based on negative theoretical view of men of this kind tend to perform relatively poorly compared to more standard therapies.
It is much more likely that men will benefit from therapies that are truly male-centered. That is, not merely adopting a male-friendly approach on a superficial level (e.g. earthy language, not explicitly focused on feelings) but being unambiguously male-centred in the sense of Carl Rogers’ idea of person-centred therapy, summarised by three factors:
Unconditional positive regard: therapists should be accepting and non-judgemental;
Congruence: therapists should be open with the client about their view of men and masculinity e.g. whether they think gender norms are a significant cause of men’s problems or not;
Empathy e.g., if your client doesn’t think patriarchy caused his marriage breakdown, best to work with him on that basis.
Note that it is not enough merely to say ‘masculinity isn’t toxic’, yet simultaneously claim that masculine norms are problematic, because both positions are negative about masculinity. This is a problem because both characterisations of masculinity distract from the real issues facing men and boys (such as the absence of fathers from homes), and there is evidence that men who think masculinity has a negative impact on them have worse mental wellbeing.
It has become popular to blame masculinity in one way or another for men’s problems e.g. masculinity is a barrier to men seeking help. However although the literature connecting masculinity to mental health is in abundance, the evidence is surprisingly weak. For example, one widely-cited paper called 'Masculinity and suicidal thinking' (Pirkis et al, 2017) found that ‘masculinity’ was only the fifth most strongly correlated variable with suicidality. Moreover it was only barely statistically significant, and in fact used a very narrow definition of masculinity (based on one masculinity subscale comprising two questions about refusing to seek help). Other research linking masculinity to suicidality and mental health problems is almost invariably similarly weak, though most people don’t seem to realise this, and cite the research uncritically.
There tends to be less empathy for some male-typical issues e.g. a man distressed about a false accusation of sexual abuse being made against him, or a man going through divorce or struggling to find access to his children etc. The list goes on. Partly the reason for the lack of empathy is due to the fact that around 80% of therapists are women, so don’t have lived experience of these issues. It is likely that there is a certain amount of cognitive distortion around gender issues which means that problems impacting men are taken less seriously than problems facing women. This cognitive distortion is suggested to be common in the social sciences and therapy field where therapists are educated and trained, and the view of men e.g. hegemonic masculinity, patriarchy theory, tend to be relatively unsympathetic to men.
Gaps in data or evidence
Benefits of masculinity
People tend to focus on problems with masculinity, but ignore potential benefits of masculinity despite the fact that there is evidence that traditional masculinity is linked to better mental health e.g. one study found that higher self-esteem and mental positivity were predicted by more acceptance of traditional masculinity. Interestingly, when researchers happen to find benefits of masculinity the findings risk being ignored or dismissed. For example, a systematic review found masculinity was beneficial for men in their 40s in coping with depression. However the systematic review dismissed the papers that found this, claiming such information might put “pressure on men to meet hegemonic ideals [and] reproduce traditional gender relations and power imbalances”. This claim demonstrates the closed and negative mindset of many researchers, which has been described as ‘paradigm fixation’.
Benefits of male-centred therapy
It is suggested that typical modes of therapy are female-centred. Men tend to seek therapy less than women do, and perhaps they would opt for a male-centred option if such was available. There is a severe lack of research evidence on whether a male-centred therapy would (a) appeal more to men and (b) work better for men than treatment as usual.
[END OF SUBMISSION TO THE UK GOVERNMENT’S MEN’S HEALTH STRATEGY]
So that was the submission from the Centre for Male Psychology. It's been four months since the submission deadline closed, and it has been stated in the House of Lords that“we intend to develop and publish the Strategy by the end of 2025”. As far as I know no definite date has been set for this, but it makes sense for it to come out during November, which is increasiningly widely recognised as Men’s Health Month.
While we wait for the publication of the Men’s Health Strategy, we might reflect on the fact that the call for evidence, unlike some previous calls for evidence, hasn’t been followed with subsequent open discussions among experts, or presentations of evidence orally in Westminster. This means the review of submitted evidence, such as the one above from the Centre for Male Psychology, has been handled entirely behind the closed doors of the Department of Health and Social Care (DHSC), with data processing, analysis, and synthesis conducted by the Men’s Health Strategy policy team of the Civil Service. Arguably the importance placed on DEI in the Civil Service lends it to being more likely to see men as privileged rather than needing help, but I hope the outcome will be better than the outcome of the UK government inquiry on the mental health of boys and men, which started out well and gathered some very good evidence, but ended up being derailed into gender ideology, and eventually - perhaps mercifully - fizzled out into nothing. The present strategy is being done in partnership with Movember, an organisation which has earned a great deal of enthusiastic support over the years, though more recently has been criticised for having become too influenced by feminism. So although there is no guarantee this, or any, call for evidence will produce something that will be of fullhearted benefit to men, let’s live in hope and not presume the outcome before we see the report.
[Update 19th Nov 2025: today, International Men’s Day, the UK government released it’s strategy report. From an initial glance it looks like they have ignored the advice of the Centre for Male Psychology, and are basing their policy around the idea that masculinity - or ‘societal norms associated with being a man’ as they call it - is a problem for men’s health. The report says “To address current societal norms associated with being a man and that lead to poor health and wellbeing outcomes, we are implementing the recently updated guidance on RSE and health education in schools”. Those of you who know how RSE and similar lessons tend to play out in schools will realise that the government has not taken good advice in creating their health strategy.]
Disclaimer: This article is for information purposes only and is not a substitute for therapy, legal advice, or other professional opinion. Never disregard such advice because of this article or anything else you have read from the Centre for Male Psychology. The views expressed here do not necessarily reflect those of, or are endorsed by, The Centre for Male Psychology, and we cannot be held responsible for these views. Read our full disclaimer here.
Like our articles?
Click here to subscribe to our FREE newsletter and be first
to hear about news, events, and publications.
Have you got something to say?
Check out our submissions page to find out how to write for us.
.