Male Depression: The Centre for Male Psychology's Position Statement on Identifying, Understanding, and Treating Men's Experiences of Depression
CLICK HERE to download the PDF version of this document.
Executive summary
Depression in men is under-recognised, under-diagnosed, and often manifests differently in men than in women. Men are less likely than women to seek help, more likely to externalise symptoms (e.g., aggression), and self-medicate (e.g., alcohol abuse).
The Centre for Male Psychology is committed to advancing evidence, improving clinical practice, and influencing public discourse on men’s mental health (Centre for Male Psychology, 2021). In this position statement we recommend a male-centred approach to understanding male depression. We hope that this document will bring about a change in how we research, treat, and talk about men’s depression.
1. Introduction and Rationale
Women are around twice as likely to be diagnosed with severe depression than men are (Albert, 2015). This disparity has, understandably, led to a focus on depression in women rather than in men across Western and non-Western cultures. In recent times, there has been a growing belief that depression in men is under-recognised, under-diagnosed, and often manifests differently in men than in women (Talarowska et al., 2018). Traditional diagnostic approaches may miss male-pattern depression, leading to misdiagnosis or no diagnosis (Zierau et al., 2002).
Identifying male depression
Most people, including clinicians, tend to think of depression as it presents in women, that is, low mood, crying, and a tendency to talk about feelings as a way of dealing with this (Morison et al., 2014). However, men may express depression through irritability, risk-taking behaviours and substance abuse, somatic issues such as insomnia, or social withdrawal (Barry et al., 2023). Some researchers have found that depression in men is more likely to manifest in the form of externalizing symptoms such as irritability, anger, extreme risk-taking, substance abuse, or impulsivity (Addis, 2008) (Von Zimmermann et al., 2024). When (Martin et al., 2013) a depression screening questionnaire was modified to include questions on these externalizing symptoms, the sex differences in depression rates disappeared (Martin et al., 2013). As our understanding of sex differences in depression continues to evolve with new research, it is important to ensure that clinical work, public policy, and future research are aligned with this information. The British Psychological Society’s Practice Briefing on Psychological interventions to help male adults (Seager & Barry, 2022) has been a useful step in that direction.
2. Core positions and principles
Sex differences should not be ignored
In recent decades, there has been a trend to downplaying average population sex differences. However, in doing so, gender-typical symptoms are overlooked, meaning treatment options are overlooked. Where they have been noted, it is often presumed that male-typical tendencies e.g. externalising behaviours, are inferior to those of females (Liddon & Barry, 2021).
This leads to two problems. First, gender-specific symptoms, as discussed above in the case of depression, are missed by practicing professionals. Second, mental health professionals end up taking a one-size-fits-all approach that may impede the treatment of individuals, especially men, who might respond better to a different, more male-centred approach to therapy.
Understanding male depression
This lack of curiosity regarding sex differences, combined with the tendency to see masculinity as a deficit, has led to an impoverished and unrealistic view of the mental life of men.
Explanations for men’s behaviour based on ideas such as patriarchy theory and hegemonic masculinity are widespread, but these are a distortion of reality. Intentionally or unintentionally, these theories create a negative ‘deficit’ view of masculinity suggesting, for example, that the high suicide rates in men is a consequence of masculinity. These negative views of men probably contribute to the lack of empathy and lack curiosity regarding issues like the underdiagnosis of depression in men. Furthermore, ideas like patriarchy theory and hegemonic masculinity are likely to impede a therapist's ability to properly understand men and build an effective therapeutic alliance (Liddon & Barry, 2021).
In contrast to the prevailing negative views of masculinity, research on the relationship between masculinity and depression in men shows reasons to be positive about masculinity. A meta-analysis of 58 papers by (Lin et al., 2021) found that masculinity traits are a protective factor against depression. Similarly, a meta-analysis of 23 studies found that traditional masculinity can be a useful resource for middle-aged men coping with depression (Krumm et al., 2017). The claim that masculinity is a barrier to help seeking is exaggerated in relation to suicidality (Barry, 2025a), and an exaggeration in relation to physical and mental health issues (Liddon & Barry, 2021), due in part to research that samples college-age men rather than more mature men.
Rather than attempting to explain male depression as a result of masculinity, the social factors that can precipitate a depressive episode in men need to be recognised, such as family breakdown, relationship breakdown, work issues, domestic violence, or legal problems such as false allegations of abuse (Liddon & Barry, 2021). Stressful events may lead to behaviours that are considered disorders in their own right, such as substance use, sex addiction, excessive gambling, or excessive online gaming, but these in some cases might best be seen as manifestations of an underlying depression (Barry et al., 2023).
Treating male depression
It is a common assumption that the role of a counsellor and the counselling process in itself is a neutral approach. However, a study by (Morison et al., 2014) titled “Are mental health services inherently feminized?” found that the therapy process, considered neutral, is more congruent with female styles of communication and emotional processing than male styles e.g. therapy typically focuses more on talking about feelings, whereas men might prefer a more solution-focused approach or an approach that reframes help-seeking as the rational course of action towards self-improvement (Liddon et al., 2019).
Research (McGrath et al., 2022) has shown that community-oriented interventions such as Men’s Sheds, sports-related interventions, or behavioural activation can be used to account for men’s preferences for concrete language, focus on action, and therapeutic alliance building (McGrath et al., 2022). A scoping review also reported improved help-seeking behaviour in men when action-oriented interventions like soccer, group, and community building were used (Kim & Yu, 2023).
In contrast to the ‘deficit’ model of masculinity, a new ‘strength-based’ or ‘positive’ approach to masculinity is emerging in the literature on men’s mental health. An example of this positive approach is the Positive Psychology/Positive masculinity Framework developed by (Kiselica & Englar-Carlson, 2010). Much like the positive psychology paradigm (Seligman, 2002), the positive masculinity framework focuses on the positive aspects of masculinity such as heroism, self-reliance and action-orientation. The strengths-based approach has shown promise in initial research (Kiselica, 2008) though further research is needed to identify how best it can be implemented across different cultures and age groups.
Mental health care providers also need to be alert to social factors that can precipitate a depressive episode in men, such as family breakdown, mentioned in the section on understanding male depression. They should similarly be vigilant to subtle signs of distress, such as substance abuse, that can be linked to suicidality.
Tailored Interventions and Adaptations
There is a strong argument to be made that adapting psychological interventions for men will improve outcomes in mental health. There is evidence that male-friendly therapy and/or strengths-based interventions are beneficial to men (Kiselica, 2008); McGrath et al., 2022; Boerma et al., 2024). Training mental health providers in these modalities and offering them to male clients as a part of routine care could improve rates of help-seeking and dropout rates, and potentially improve therapy outcomes for men too.
A distinction should be made between male-friendly therapy and male-centred therapy. Male-friendly therapy can involve embedding simple techniques such as humour/banter and a shoulder-to-shoulder communication style, as well as solution-focused and action-orientated approaches, and community-based interventions, among others. (Liddon et al., 2019). A narrative review the characteristics of male-friendly therapy concluded that empathy is central to this approach (Liddon et al., 2019). There is however a more superficial interpretation of a male-friendly therapy where, for example, language that appeals to men is used, but the underlying view that masculinity is a part of the client’s problem remains (Barry, 2025b). It is suggested that a more thoroughly male-centred approach is needed, based on the Rogerian model (Rogers, 1951). This male-centred approach emphasises -that in addition to the recommendations of (Liddon et al., (2019) that congruence and unconditional positive regard are key pillars of therapy with men (Barry, 2025b).
Efforts should be made to find situations and factors that make men comfortable, such as improving the therapeutic alliance, adopting positive attitudes towards masculinity, and helping men develop positive internal narratives about masculinity (Barry, 2023). It is possible that some cases of male depression may be related to having internalised negative narratives about masculinity (Barry, 2023), which in theory could lead to a state of ‘gender alienation’ (Seager & Barry, 2019). Examples of negative narratives are toxic masculinity, hegemonic masculinity, patriarchy theory, or the idea that ‘traditional masculinity’ is harmful to physical and mental health. Although many men will have already reality-tested the validity of patriarchy theory against the many disadvantages facing men (Seager & Barry, 2019), some men may be more invested in negative theories about men, in which case the therapist should aim to gently move such clients towards a more accepting self-concept.
Preventive and Public Engagement Work
While clinicians can play an important role in helping men overcome depression, actually reaching men who need help requires interventions at a public and policy level.
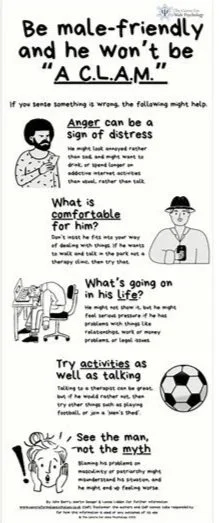
Figure 1. Infographic from the Centre for Male Psychology’s ‘A. C.L.A.M.’ mental health awareness campaign.
The Centre for Male Psychology supports developing community, workplace, and media programs to raise awareness on issues related to men’s mental health and men’s depression. This can be done in the form of plays, shows, outreach workshops, and other engaging activities that educate the public. It is essential that these programs focus on psychoeducation and raising awareness of the symptoms of male depression. An example is the Centre for Male Psychology campaign in 2023, which used an infographic (Figure 1) to illustrate the signs of distress in men, and what can be done to alleviate it (Barry et al., 2023). To maximise the impact of the campaign, it was designed to be easy to understand (jargon-free language) easy to remember (based around images and an acronym), and included an additional informational section aimed at mental health professionals.
A common narrative in the context of men’s mental health is that men don’t seek help often enough or don’t ‘open up’. We don’t believe this narrative is helpful in the long run. This belief utilizes a monocausal explanation that puts the ‘blame’ of underutilization of mental health services solely on the shoulders of men (Whitley, 2021). It is unhelpful to expect men to open up when doing so leaves them feeling awkward and misunderstood. In a survey of more than 4000 young men, 41% reported they regretted opening up to others (Movember, 2019). Instead, the focus should be shifted from men needing to open up, to adapting mental health services in a way that men feel ready to participate in.
Research and Evidence Integration
While there is increased interest in the mental health of boys and men, depression in men continues to be significantly under-researched. We advocate for funding and conducting high-quality research on male-specific depressionogenic pathways, and for safe and effective interventions with positive long-term outcomes. These will include randomised controlled trials (RCTs) comparing male-centred therapies with a variety of treatments-as-usual (TAU) rather than just waiting-list control groups. Such studies will help us test and improve the efficacy of male-centred therapies and with the goal of making them ready for implementation in everyday practice.
An integrated and evidence-driven approach to improving the mental health of men requires sincere collaboration across multiple stakeholders. We support continuous assessment of treatment safety and efficacy, with service evaluations and open communication between practitioners, researchers, and policy makers.
3. Stated Position
The current gender-blind approach to men’s mental health does not seem to have reduced depression rates or suicide rates in men. In fact, the current approach may be underdiagnosing men who need urgent care. It is imperative to explore alternative options.
The current models of depression and its treatment have proven insufficient for male clients. These approaches are apparently gender-neutral or implicitly female-oriented or based on a deficit model of masculinity, none of which are helpful for male clients. It is essential to train mental health practitioners in male psychology and develop competence in applying this knowledge to the therapeutic context (Centre for Male Psychology, 2025)
We reject any framing that pathologizes masculinity. Instead, we see masculinity as a resource that can be nurtured and may protect against depression or help reduce it (Barry et al., 2020). Research has consistently shown that the therapeutic alliance is the cornerstone of therapy, and a male-centred perspective should help develop a fruitful relationship between the therapist and the client.
Suggestions that masculinity is problem because it is ‘rigid’ only makes sense in terms of the Rational Emotive Behaviour Therapy (REBT) framework, where any belief can be a problem if held too rigidly. But the solution, according to REBT, is to reduce the rigidity of the belief, not to undermine the belief itself (Liddon & Barry, 2021). The success of REBT as a treatment also highlights the benefits of stoicism (Ellis, 1979), in contrast to popular claims linking stoicism to a deficit view of masculinity.
There is an unfortunate paucity of research on sex differences in outcomes of therapy for depression, especially longitudinal studies. We call on psychological professional bodies, mental health services, and funding agencies to prioritise male depression. Existing therapeutic modalities should be tested against new male-centred modalities, collecting sex-disaggregated data on outcomes. Satisfactory results will highlight the need for offering flexible services to male clients suffering from depression, and training clinicians in male-centred approaches.
4. Recommendations and Calls to Action
For Clinicians and Services
Clinicians and mental healthcare providers are encouraged to undertake training in understanding men and masculinity from a male-centred perspective. Understanding men better will help them create an effective therapeutic alliance. A stronger therapeutic alliance may prevent high rates of dropout from therapy and improve therapy outcomes (Whitley, 2018).
Clinicians are also encouraged to offer therapy modalities that are more appealing to men with a focus on an action-orientation or a community support system, such as sports-related interventions, Men’s Sheds, and solution-focused therapy. Clinicians can also incorporate elements of therapy that increase chances of engagement from men, such as shoulder-to-shoulder communication, shared activities, and a positive view of masculinity.
We strongly encourage mental health providers to look out for male presentations of depression and routinely screen for male-typical depression.
For Researchers
Men’s mental health, especially men’s depression, continues to be under-researched. We encourage more and better research into the sex differences in outcomes of different therapy modalities. Understanding how different modalities affect the sexes differently will help us develop better interventions for men and women. It will also important to report changes in outcomes relevant to male depression, such as changes in irritability, improvement in opinions on masculinity, and changes in anger outbursts.
It is important to investigate barriers to help-seeking in male populations across cultures, ages, and ethnicities. These investigations must not be restricted to the narrow assumption that reduced help-seeking is caused by men fearing that seeking help makes them look weak.. If attempts are made to understand the role masculinity plays in help-seeking, the definition of masculinity should be realistic, and not based on the deficit model.
Future research can also break new ground by investigating the impact of depictions of men and masculinity on various outcomes in men and boys. For example, the effect of depictions of men in the media on the self-esteem of boys, the impact of masculinity school workshops on boys’ self-esteem, and the degree to which negativity about masculinity alienates males from a healthy sense of their masculinity (gender alienation). The more we understand men, the better equipped we will be to help them.
Sex differences may be of clinical relevance, so clinical trials should include women where possible and appropriate. The findings of sex differences research may be of use to men and women alike. It will be found that some women are more male-typical in some respects, in which case they may benefit from therapy orientated towards men.
Long-term follow up is essential, as this may reveal sex differences not detected by simple pre-post designs (Wright & McLeod, 2016).
For Policymakers and Funders
Policymakers and research funders can shape the future of men’s mental health with their influence on public discourse and funding new initiatives. We encourage policymakers to support research into understanding the causes of depression in men and boys instead of simply assuming the causes are uniform across genders, or are related to defects in masculinity.
Research funds can also be directed towards services tailored for men and their cultural realities, such as male-specific helplines and community outreach programs encouraging men to seek help for their mental health. It is also important to organize public programs in workplaces, the media, and in educational institutions to target men’s mental health and make it a priority in the public discourse on men’s mental health.
As more research is carried out on mental health programs and their effectiveness, special attention should be paid to the uptake of these services for men, what barriers they face, and the therapeutic outcomes they experience. This will help ensure that not only are the treatments safe and effective, but are sought by men, and once signed up to, men will complete the full course of treatment.
Final Statement
Men’s depression is a serious public health concern that is often misunderstood as a problem caused by masculinity. The Centre for Male Psychology stands firmly for approaches that combine scientific rigour with gender competence. To reduce the human cost of untreated depression in men, we must re-examine practice, policy, and public narrative.
If you or a man you know is experiencing mental health issues, you can find help and advice on the Centre for Male Psychology support page here.
References
Addis, M. E. (2008). Gender and depression in men. Clinical Psychology: Science and Practice, 15(3), 153–168. https://doi.org/10.1111/J.1468-2850.2008.00125.X
Albert, P. R. (2015). Why is depression more prevalent in women? J Psychiatry Neurosci, 40(4), 219. https://doi.org/10.1503/jpn.150205
Barry, J. (2023). The belief that masculinity has a negative influence on one’s behavior is related to reduced mental well-being. International Journal of Health Sciences, 17(4), 29–43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10321463/
Barry, J. (2025a, September 10). It’s time to change the narrative about masculinity and suicide: World Suicide Prevention Day 2025 — The Centre for Male Psychology. Male Psychology. https://www.centreformalepsychology.com/male-psychology-magazine-listings/its-time-to-change-the-narrative-about-masculinity-and-suicide-world-suicide-prevention-day
Barry, J. (2025b, October 8). Building a healthier future for men’s mental health: The case for male-centred therapy — The Centre for Male Psychology. Male Psychology. https://www.centreformalepsychology.com/male-psychology-magazine-listings/building-a-healthier-future-for-mens-mental-health-the-case-for-male-centred-therapy
Barry, J., Seager, M., & Liddon, L. (2023, November 19). ‘Men won’t CLAM up if you’re male-friendly!’ A brief guide to supporting men’s mental health. Male Psychology, 4,3, 1–11. https://www.centreformalepsychology.com/male-psychology-magazine-listings/men-wont-clam-up-if-youre-male-friendly-a-brief-guide-to-supporting-mens-mental-health
Barry, Walker, Liddon, & Seager, M. J. (2020). Reactions to contemporary narratives about masculinity: a pilot study. Psychreg Journal of Psychology, 4(2), 8–21.
Boerma, M., Beel, N., & James, N. (2024). Male-friendly counselling for young men: a thematic analysis of client and caregiver experiences of Menslink counselling. Australian Psychologist, 59(6), 496–507.
Centre for Male Psychology. (2021). About The Centre For Male Psychology — The Centre for Male Psychology. https://www.centreformalepsychology.com/about-the-centre-for-male-psychology
Ellis, A. (1979). Is Rational-Emotive Therapy Stoical, Humanistic, or Spiritual? Journal of Humanistic Psychology, 19(3), 89–92. https://doi.org/10.1177/002216787901900314
Kim, S., & Yu, S. (2023). M I N I-R E V I E W Men’s mental health and interventions tailored to masculinity: a scoping review. 19(11), 1–10. https://doi.org/10.22514/jomh.2023.111
Kiselica, M. S. (2008). When Boys Become Parents: Adolescent Fatherhood in America. Rutgers University Press. https://books.google.co.uk/books?id=PaM84_v4oGwC
Kiselica, M. S., & Englar-Carlson, M. (2010). Identifying, affirming, and building upon male strengths: the positive psychology/positive masculinity model of psychotherapy with boys and men. Psychotherapy Theory, Research, Practice, Training, 47, 3, 276–287. https://psycnet.apa.org/record/2010-20923-002
Krumm, S., Checchia, C., Koesters, M., Kilian, R., & Becker, T. (2017). Men’s Views on Depression: A Systematic Review and Metasynthesis of Qualitative Research. Psychopathology, 50(2), 107–124. https://doi.org/10.1159/000455256
Liddon, L., & Barry, J. A. (2021). Perspectives in Male Psychology: An Introduction. Wiley. https://www.wiley.com/en-gb/Perspectives+in+Male+Psychology%3A+An+Introduction-p-9781119685357
Liddon, L., Kingerlee, R., Seager, M., & Barry, J. A. (2019). What Are the Factors That Make a Male-Friendly Therapy? In J. A. Barry, R. Kingerlee, M. Seager, & L. Sullivan (Eds.), The Palgrave Handbook of Male Psychology and Mental Health (pp. 671–694). Springer International Publishing. https://doi.org/10.1007/978-3-030-04384-1_32
Lin, J. ;, Zou, L. ;, Lin, W. ;, Becker, B. ;, Yeung, A. ;, Cuijpers, P. ;, Li, H., Lin, J., Zou, L., Lin, W., Becker, B., Yeung, A., Cuijpers, P., Li, H. (, Lin, J., Zou, L., Lin, W., Becker, B., Yeung, A., & Cuijpers, P. (2021). Does gender role explain a high risk of depression? A meta-analytic review of 40 years of evidence Does gender role explain a high risk of depression? A meta-analytic review of 40 years of evidence. Journal of Affective Disorders, 294, 261–278. https://doi.org/10.1016/j.jad.2021.07.018
Martin, L. A., Neighbors, H. W., Griffith, D. M., & Psychiatry, J. (2013). The Experience of Symptoms of Depression in Men vs Women Analysis of the National Comorbidity Survey Replication Supplemental content at jamapsychiatry.com Original Investigation. https://doi.org/10.1001/jamapsychiatry.2013.1985
McGrath, A., Murphy, N., Egan, T., & Richardson, N. (2022). Sheds for life: health and wellbeing outcomes of a tailored community-based health promotion initiative for men’s sheds in Ireland. https://doi.org/10.1186/s12889-022-13964-6
Morison, L., Trigeorgis, C., & John, M. (2014). Are mental health services inherently feminised? The Psychologist, 27(6), 414–416.
Movember. (2019). Perceptions of Masculinity & the Challenges of Opening Up. https://cdn.movember.com/uploads/images/2012/News/UK%20IRE%20ZA/Movember%20Masculinity%20%26%20Opening%20Up%20Report%2008.10.19%20FINAL.pdf
Rogers, C. (1951). Client Centred Therapy. Constable.
Seager, M., & Barry, J. (2022). Practice Briefing on Psychological interventions to help male adults . https://cms.bps.org.uk/sites/default/files/2022-11/Practice%20Briefing%20-%20psychological%20interventions%20to%20help%20male%20adults.pdf
Seager, M., & Barry, J. A. (2019). Cognitive Distortion in Thinking About Gender Issues: Gamma Bias and the Gender Distortion Matrix. The Palgrave Handbook of Male Psychology and Mental Health, 87–104. https://doi.org/10.1007/978-3-030-04384-1_5
Seligman, M. E. P. (2002). Positive Psychology, Positive Prevention, and Positive Therapy. In C. R. Snyder & S Lopez (Eds.), Handbook of positive psychology, (pp. 3–12). Oxford University Press, Inc.
Von Zimmermann, C., Hübner, M., Mühle, C., Müller, C. P., Weinland, · Christian, Kornhuber, J., & Lenz, · Bernd. (2024). Masculine depression and its problem behaviors: use alcohol and drugs, work hard, and avoid psychiatry! 274, 321–333. https://doi.org/10.1007/s00406-023-01567-0
Whitley, R. (2018). Men’s Mental Health: Beyond Victim-Blaming. The Canadian Journal of Psychiatry, 63(9), 577–580. https://doi.org/10.1177/0706743718758041
Whitley, R. (2021). Men’s Issues and Men’s Mental Health: An Introductory Primer. Men’s Issues and Men’s Mental Health: An Introductory Primer, 1–255. https://doi.org/10.1007/978-3-030-86320-3/COVER
Wright, K., & McLeod, J. (2016). Gender difference in the long-term outcome of brief therapy for employees. New Male Studies, 5(2), 88–110.
Zierau, F., Bille, A., Rutz, W., & Bech, P. (2002). The Gotland Male Depression Scale: A validity study in patients with alcohol use disorder. Nordic Journal of Psychiatry, 56(4), 265–271. https://doi.org/10.1080/08039480260242750
Disclaimer: This article is for information purposes only and is not a substitute for therapy, legal advice, or other professional opinion. Never disregard such advice because of this article or anything else you have read from the Centre for Male Psychology. The views expressed here do not necessarily reflect those of, or are endorsed by, The Centre for Male Psychology, and we cannot be held responsible for these views. Read our full disclaimer here.
Like our articles?
Click here to subscribe to our FREE newsletter and be first
to hear about news, events, and publications.
Have you got something to say?
Check out our submissions page to find out how to write for us.
.