Workplace mental health schemes must address men’s needs

Anything that moves us toward a greater understanding of mental health is to be welcomed. Recently, the Heads Together organisation has partnered with a number of other groups to develop the Mental Health at Work site.
There are many resources on this site and it is a good start towards what Heads Together call “Changing the conversation and tackling the stigma around mental health”. We know that job satisfaction is a major factor in men’s wellbeing, but how much do programmes such as the Mental Health at Work site take men’s needs into account, especially the mental health needs of working class men?
We know that not all programmes aimed at supporting mental health at work are equally effective for men and women. For example, one large study found that when counselling was provided in an EAP (Employee Assistance Programme), only women continued to benefit in the long term, suggesting that men and women may differently experience and benefit from mental health interventions.
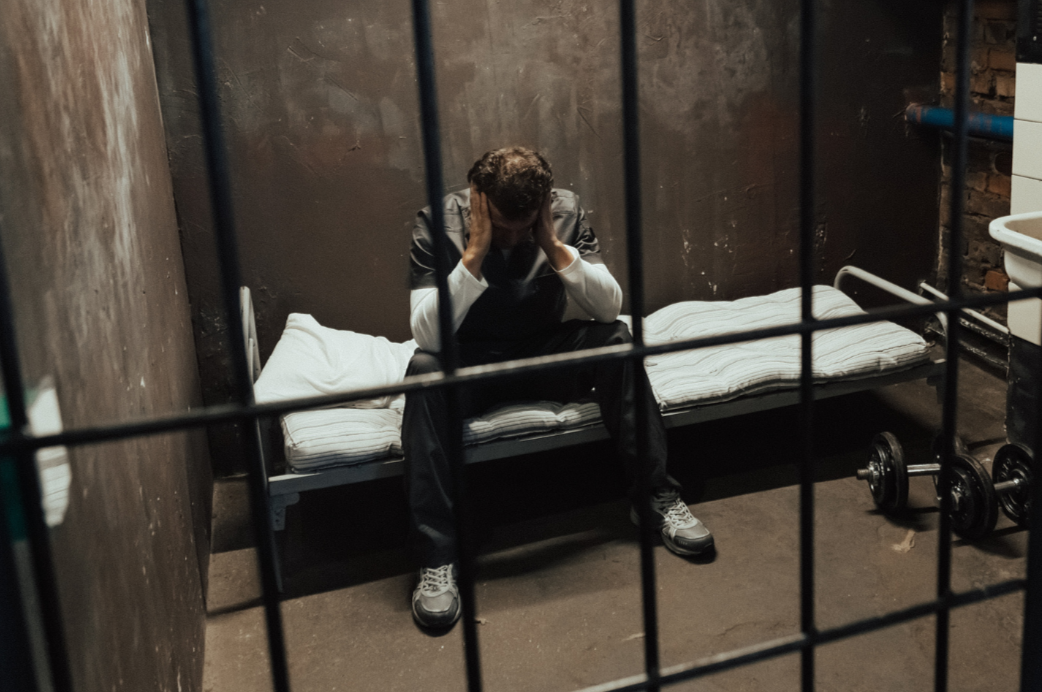
Men tend to be the workers in heavy industry and jobs requiring the most hard physical labour, and women are more likely to gravitate to more people-orientated work. How might the gender difference in job choice be relevant to mental health? Mental health problems can lead to poor performance, absenteeism, workers being fired and even workplace accidents and deaths. As I outlined at the 2018 Male Psychology Conference in University College London, workplace deaths are highly skewed towards men. This is partly attributable to men doing more dangerous jobs, but it is perhaps also attributable to EAPs not successfully addressing men’s particular perspectives and needs in regards their mental health.
Men often invest a great deal of themselves in their work, and in the importance of doing a good job. While perhaps there may be a need to balance this with family responsibilities, we should consider that it might be best if workplace mental health programmes respond to the way men actually are, not how we think they should be. Unemployment is more predictive of suicide risk in men than women, which suggests that extra care should be taken in EAPs for men who have concerns about unemployment. As we know, suicide figures are grossly distorted towards men, usually putting them at about 75% of all people dying by suicide.
Men can be relatively poor at reaching out for help, but services provided for them need be presented – in terms of marketing channels used – and operated according to how men typically talk, behave and act. If we want to reduce the number of direct and indirect workplace deaths, which may be due to poor risk decision-making caused by mental illness, stress and untreated physical ailments, then we have to provide programmes which attend to the particular needs of men, and women too. More research is needed on how to achieve more effective gender sensitivity in EAPs.
Since in general men tend to prefer a solution-focused step by step approach and women tend to prefer to talk about their feelings, this should inform the real-life and hypothesised examples provided, both in text and in acted out role play examples in online videos. It is important to provide something concrete, particularly for men, so that those who have not had mental health problems previously can see, and thus understand, what it is like to experience those problems. Finally, there could be more video testimonies of both men and women (the more high profile the better, as people respond positively to well regarded celebrity or high status role models) talking about how they came through their mental health problems and how they maintain their mental health now.
While I found much good material on the Mental Health at Work site, I felt that it could be even better if it was more designed to take gender differences in mental health and functioning at work into account. The steps towards recognising their problem (e.g. through online self-administered tests), case studies (going from experience through diagnosis to recovery) and to how to access mental health services, can all be improved by adapting future versions of the Mental Health at Work site to the different needs often seen in men and women.
This article was first published on the Male Psychology Network website in 2018
Scroll down to join the discussion
Disclaimer: This article is for information purposes only and is not a substitute for therapy, legal advice, or other professional opinion. Never disregard such advice because of this article or anything else you have read from the Centre for Male Psychology. The views expressed here do not necessarily reflect those of, or are endorsed by, The Centre for Male Psychology, and we cannot be held responsible for these views. Read our full disclaimer here.
Like our articles?
Click here to subscribe to our FREE newsletter and be first
to hear about news, events, and publications.

Have you got something to say?
Check out our submissions page to find out how to write for us.
.
Dr Joe MacDonagh is a Chartered Psychologist, a Chartered Scientist and is a former President of the Psychological Society of Ireland – the professional body for psychologists in Ireland. He is also a former Chair of the Irish Academy of Management and is currently Honorary Secretary of the History and Philosophy of Psychology section of the British Psychological Society.