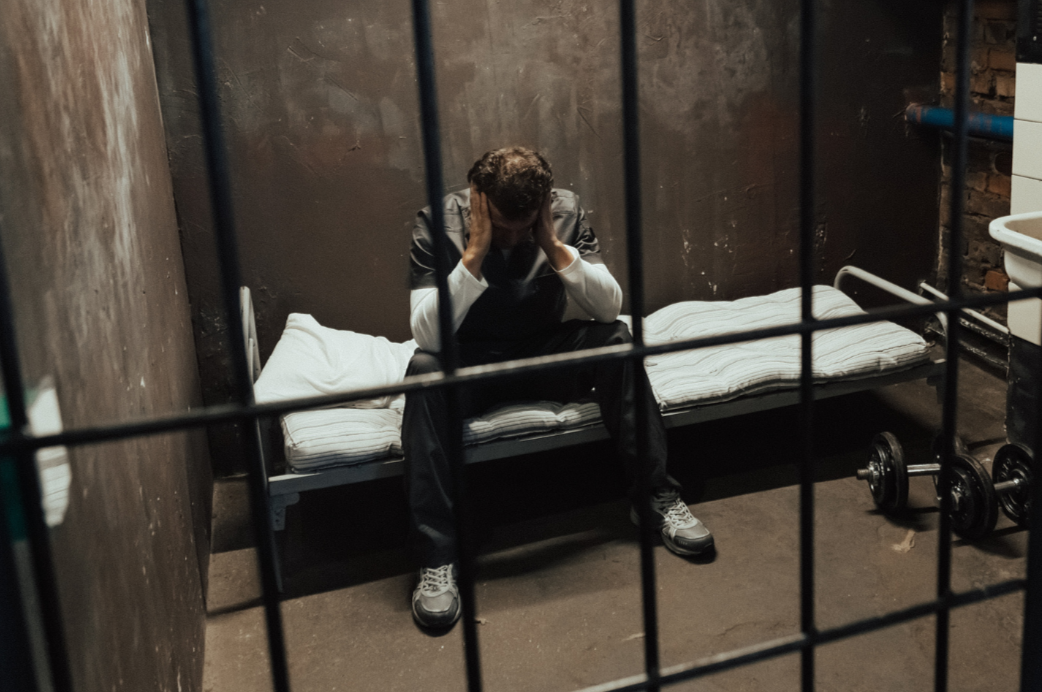
A success story for men’s mental health: Therapist Andy Noon discusses James’ Place, a charity saving the lives of men in suicidal crisis
In 2006, beset by anxiety and suicidal thoughts, a young man called James Wentworth-Stanley took his own life. His parents were determined to create something that meant other families wouldn’t experience a similar loss, so they founded James’ Place, a friendly non-clinical centre where suicidal men are offered quick access to professional therapy without any fee being charged. The first James’ Place opened in Liverpool in 2018, followed by a London centre in 2022, then one in Newcastle in 2024.
Andy Noon has worked in healthcare since 2012, and in 2023 became the Head of Centre for James’ Place Liverpool. I was keen to find out from Andy what makes James’ Place unique, and about his role there.
John Barry (JB): You’ve recently joined James’ Place Liverpool as their Head of Centre which sounds a great opportunity. Your role includes managing your team as well as providing treatment to men in suicidal crisis. Can you give an insight into a typical day at work?
Andy Noon (AN): My day is usually spent half delivering therapy sessions myself to the men that use our service, and half managing the team of therapists and speaking to our partners and referrers. In a typical day I’d review the referrals that have come in with the senior therapist in the team, making a judgement as to whether we can support that person, if we are the right service for them. I then might have a therapy session with one of my caseload of men I’m supporting or a welcome assessment with a new man to the service. I’d then be supporting and line managing my team of therapists and centre manager, making sure they are happy and supported, dealing with any problems they might have, looking at any safeguarding issues. Also part of my role is outreach, attending local events in the community and building relationships so that people know about our service and who we can support.
“We use a set of cards with different thoughts, emotions, feelings, scenarios on them to quickly help men articulate why they are in a suicidal crisis, what is keeping it going and how they might get out of it.”
JB: If a man is struggling, how can he or his family get help from one of James’ Place Centres? Can he just turn up or is there a process and criteria for referral?
AN: We treat men in suicidal crisis and by that we mean a man is experiencing intense and distressing suicidal thoughts which they plan to act on. We are an appointment-only service and men can self-refer or be referred to us by a professional including those working in health and community services, or by a friend or family member. We do have criteria which is that you need be a man or identify as male, be 18+, be registered or eligible for registration with a GP, and be willing to engage with talking therapy. The first step is going to our website and filling in a referral form at https://www.jamesplace.org.uk/get-support/ and we will get back to you within one working day.
“Our treatment is independently evaluated, and men experience a clinically and statistically significant positive change […] our treatment is successful is because it is specifically designed for men”
JB: “James’ Place saves the lives of men in suicidal crisis”. Can you describe what this life-saving treatment to suicidal men looks like, how it works and why it’s successful?
AN: Our treatment is one to one talking therapy which takes place at our warm and welcoming, non-clinical centres. Usually it comprises six to eight face to face sessions with one of our trained therapists over the course of around a month. We use a set of cards with different thoughts, emotions, feelings, scenarios on them to quickly help men articulate why they are in a suicidal crisis, what is keeping it going and how they might get out of it. We work alongside the NHS and other local support services, taking on clinical responsibility for the men we treat.
Image: Cards used by James’ Place to help men articulate why they are in a suicidal crisis'
We see men quickly with no waiting list – usually within 48 hours. Our treatment is independently evaluated, and men experience a clinically and statistically significant positive change following treatment and reduced levels of psychological distress.
The reason our treatment is successful is because it is specifically designed for men, it’s quick to access and it’s delivered face to face by a professional therapist in our centres. When developing our centres, we asked men what they would want the environment to be like and we took that on board. We wanted men to feel safe and comfortable coming to us for help, and we knew the environment would play a vital role in that.
JB: A paper by your colleagues at James’ Place (Claire Hanlon et al, 2023) notes that emerging evidence regarding help-seeking suggests that "most men had recognised their need for mental health support. However, they did not know where to go or how to ask for support." This offers a refreshingly different perspective to the received wisdom that masculinity reduces help seeking. Hanlon et al suggest making therapy more accessible to men; in what ways does James’ Place make itself visible to men and easy for them to ask for help?
AN: We work best in partnership, and we have good relationships with local crisis teams and other health services in our area to ensure they are comfortable referring men to us and that those men feel confident to come to our centres. We work in the community with local charities and community organisations to spread the word to groups they represent. We also raise awareness of our service on social media, in local media, through advertising at certain times of year. We find letting the men who have used our service tell their story works particularly well, as men feel reassured that we have helped someone they can relate to in some way. We also feel that because our service is specifically for men that helps, as we know services designed for all genders are mainly used by women. Our aim is to make it as easy as possible for men to come to us for help by removing as many barriers to them coming as we can.
“Whilst the reasons for a suicidal crisis can be complex, the main drivers for the men we see are a life event such a relationship breakdown, financial problems or bereavement.”
JB: Understandably the suicidal crisis is itself the immediate issue needing support when a man comes to one of the centres. Is there awareness of emerging themes relating to the types of issues that provide context to their current crisis (for example, relationship stress or work stress)?
AN: Whilst the reasons for a suicidal crisis can be complex, the main drivers for the men we see are a life event such a relationship breakdown, financial problems or bereavement. We know that there is a strong link between socio-economic deprivation and suicidal behaviour. Men in the lowest social class, living in the most deprived areas, are up to ten times more at risk. Of the men who came to James’ Place Liverpool in 2018-2021 82% were from areas of high socio-economic deprivation and a third were unemployed.
JB: Does James’ Place offer help with longer term issues, post therapy, such as men who have been falsely accused of a crime, or going though child custody/visitation problems?
AN: We support the man emotionally through the crisis period, helping them to access any longer-term support they might need from other services. We don’t replicate or replace existing statutory services, but instead work closely with the local NHS and wider services to ensure men are supported with any longer-term issues when they leave us.
JB: Real life experiences are often a powerful anchor to get people to take notice. Are you able to share (anonymously) any success stories of the men who pass by James’ Place?
AN: We have many success stories at James’ Place of men who have come through their suicidal crisis and gone on to lead happy and fulfilling lives. One that stands out to me is Frankie, who came to us when he was at his lowest point. He worked closely with a therapist and has since noticed a real change in himself. In fact following treatment with us he got his first ever passport at the age of 61, and now regularly sends us photos of the trips he is taking all round the world!
JB: Moving the focus to you now, you worked as a mental health nurse previously, which can be both a demanding but rewarding job. What is it about this role that appealed to you?
AN: I’ve always been a calm and compassionate person, so I felt I had the right skills for a career in mental health. It appealed to me as I was used to supporting people during very difficult times in their life. I worked as a support worker initially, supporting people in their own home with mental health needs such as psychosis and keeping them well. Finding out more about people's mental health difficulties in their life, seeing their journey and their recovery made me want to be a part of a team that would treat someone to help improve their mental health. It was also in part because of my personal experiences as well, the people who had helped me in my life inspired me to want to take on a similar role. After qualifying as a nurse and working in a number of clinical settings, I set up Evolving Mindset CIC, providing free and easy to access support for people with mild to moderate mental health needs. When I saw the role of Head of Centre for James’ Place Liverpool advertised, I knew this was the role I was destined to do. Suicide prevention is something I am passionate about and the hybrid role of both leading an exceptional team and utilising my clinical skills to provide treatment to men in suicidal crisis in Liverpool and the North West was extremely appealing to me. I feel like the service is offering a solution to support suicidal men and it’s absolutely needed in the local community.
“…it is very rewarding, seeing someone who is in such an intense period of life and then a few weeks later seeing the difference in them, and knowing you’ve helped them is an amazing feeling.”
JB: Can you tell me more about Evolving Mindset, such as what motivated you to set it up?
AN: We set up Evolving Mindset in 2019 to offer people in the community with low to moderate mental health needs free, accessible support, initially in the form of group sessions. We supported people during the pandemic and from that point it grew into a social enterprise working with organisations to deliver relevant mental health training, which then generates funds to help people in the community. Evolving Mindset has a package of support for people who might be waiting a long time for treatment or who are managed by medication in the local community, a resource for people to use other than the GP or who might feel unable to seek support from other services for a variety of reasons. The reason why we set it up is that we just heard about too many people taking their own lives and we believed that in lots of cases, something could have been done a lot earlier to prevent this.
JB: Going back to mental health nursing for a moment, in clinical psychology there tends to be more men than women (around 80%). Is it the same in mental health nursing? Do you think the ratio matters in general, or perhaps for some issues but not others?
AN: Nursing is more of a female dominated workforce, which is also true of mental health nursing although I know from my own experience that there tends to be a slightly higher percentage of male nurses working in mental health settings than in general nursing. I would like to see more men in nursing because I feel that all genders have an important part to play, and there are some occasions when it can be really useful to have a male or a female nurse in a particular situation. I do think that the workforce needs all genders, but if someone has the required skills and values then I feel they will make an exceptional nurse, regardless of their gender.
JB: What advice would you give anybody planning a career in mental health (e.g. mental health nursing, clinical psychology or other therapies, talking groups) and suicide prevention? Would you offer any specific guidance about working with suicidal men?
AN: A lot of people go into mental health in whatever capacity because they've had their own experiences or a loved one has, and they want to help others. I'd say absolutely do it, but make sure that you do your research on how demanding the job can be and think about how it might affect you emotionally especially if you have had mental health issues yourself or have lost a loved one. For example, doing a mental health nursing degree, it's three years long and half of is placement based. You’ll be in some very challenging situations during that time, you might be working nights or early mornings and you’ve got to be prepared to do that. I’d do your research, speak to people who are working within the field, get different perspectives from people and make a judgement based on that. That said, it is very rewarding, seeing someone who is in such an intense period of life and then a few weeks later seeing the difference in them, and knowing you’ve helped them is an amazing feeling.
JB: Are there any new projects in the works for yourself, or James’ Place, that you would like to share with us?
AN: We have just opened a new centre in Newcastle to help men in the North East and hope to open two more centres by the end of 2026. With five centres open half the male population in England will be within two hours of a James’ Place centre.
Final thoughts
James’ Place is based on a unique concept about helping men in mental health crisis. Proving the adage that tragedy can inspire great things, James’ Place offers men a valuable opportunity to get help when they are at their most vulnerable. Since 2018 James’ Place has treated over 1,800 suicidal men in over 7,500 therapy sessions, and there are more centres and therefore more help on the way. In a world where therapy often only comes at the end of a long waiting list, the existence James’ Place is a true lifesaver.
For more information go to www.jamesplace.org.uk
Biography
Andy Noon is from Liverpool and worked as a support worker for people with learning disabilities and mental health needs, before training as a mental health nurse in 2015. In 2022 his Community Interest Company Evolving Mindset, which has given free and easily accessible mental health support to over 2000 people, won the Merseyside Independent Health and Well-being Business of the year. He is currently Head of Centre for James’ Place Liverpool.
Scroll down to join the discussion
Disclaimer: This article is for information purposes only and is not a substitute for therapy, legal advice, or other professional opinion. Never disregard such advice because of this article or anything else you have read from the Centre for Male Psychology. The views expressed here do not necessarily reflect those of, or are endorsed by, The Centre for Male Psychology, and we cannot be held responsible for these views. Read our full disclaimer here.
Like our articles?
Click here to subscribe to our FREE newsletter and be first
to hear about news, events, and publications.
Have you got something to say?
Check out our submissions page to find out how to write for us.
.