How can we help men to be more willing to access therapy? Insights from working with prisoners

Within the UK, three times as many men kill themselves as women. Within the Republic of Ireland, this ratio rises to 5:1. Concern about male suicide, along with male over-representation in other behavioural statistics that are associated with distress (substance misuse and violence for instance) has led researchers and mental health professionals to consider whether therapy as it is currently provided is accessible to men.
Some observe that therapy is unappealing to men. Discussions of gender differences in relation to therapy suggest men find feeling-focused therapy “too woolly”, prefer structured approaches such as CBT and benefit from an approach that is made less intense by “talking whilst doing”, offering gradual exposure to emotions and with an emphasis on strength and empowerment (e.g. Seidler et al, 2017).
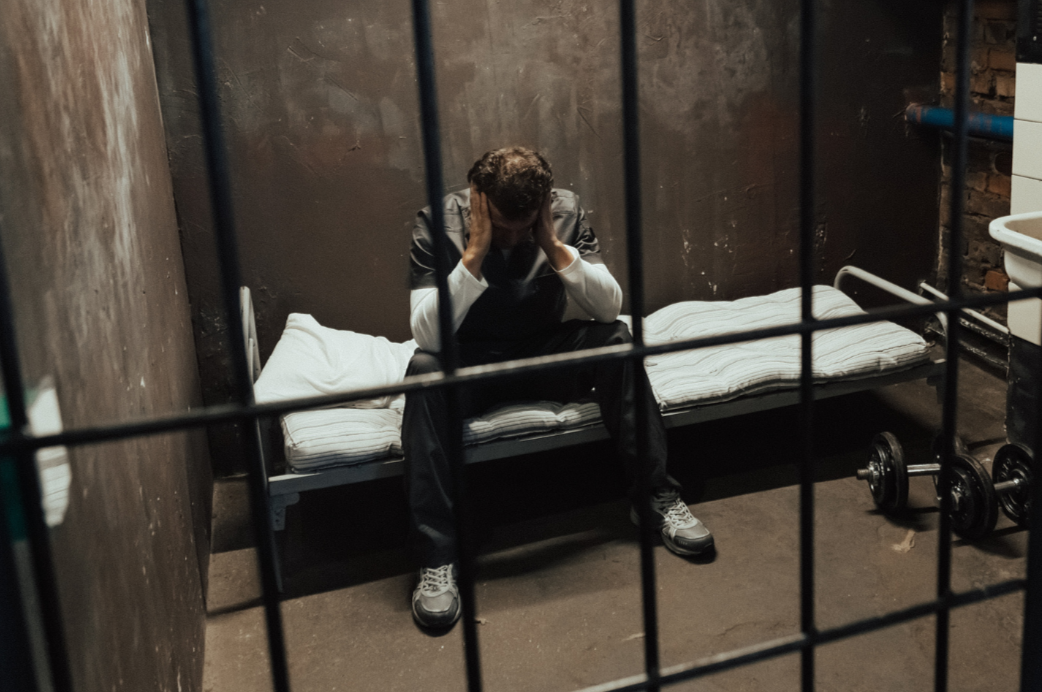
Within prison, treatment is most typically highly structured, manualised, offending behaviour programmes (OBPs). The Fens Service (HMP Whitemoor since 2000) was established for men considered to be challenging to the prison system and perceived as unable to benefit from standard OBPs. The typical service user has received a life sentence for violent or sexually violent crimes and has to some degree been labelled as “untreatable” or “treatment-resistant”. This may be because he has completed OBP treatment and is perceived as making no gains but, more commonly, he has been ejected from treatment for failing to attend regularly or turning up and being disruptive. Not infrequently, he has been unable to access treatment because his daily behaviour has proved so challenging to manage that he has been located within special accommodation that makes treatment more inaccessible. Despite this, once within the Fens Service, the average man attends 95% of the individual sessions and 88% of the group sessions available to him over the 5 year course of treatment.
Treatment is as voluntary as it can ever be when one is detained in custody. There are no immediate consequences to failing to attend a session but staff attitudes towards a D.N.A. (did not attend) may be helpful. DNA is seen as an inevitable part of beginning an emotionally intimate relationship and the struggle to establish intimacy given the context within which these men were generally raised included brutal physical and sexual abuse by multiple perpetrators in ‘care-giving’ roles, profound neglect and loss which becomes an explicit focus of discussion.
Seager & Barry (2014) highlight the importance for men of being “a fighter and winner….a provider and protector… and retaining mastery and control at all times”. Seidler et al draw the apparently logical conclusion that therapy must maintain these needs by teaching men skills and being task focused to enable the men to perhaps avoid feeling vulnerable. The approach that we utilise at Whitemoor is to normalise vulnerability as part of the human condition and to alleviate them of the burden or “shame” of asking for help by pragmatically acknowledging the hurt child that we know each of them is trying to heal. The bravery required to do this work is spoken of frequently and staff speak openly of their own emotional responses during therapy which inevitably includes feeling frightened, hated or saddened but demonstrates these feelings are not only universal but are not to be feared.
Would these prisoners have gone to therapy more readily had they been offered the ‘graded exposure’ approach suggested by authors such as Seager, Barry and Seidler? This is a moot point at present because neither approach to facilitating help-seeking has been subject to formal research. There might also be contextual and individual differences that make it difficult to compare help-seeking in the general public to help-seeking in a secure prison environment.
One thing we know is that once in treatment, the prisoners at Whitemoor have a good chance of making clinically significant improvements, so it would be very useful to know which method – graded exposure or normalising vulnerability – is more effective in encouraging prisoners to enter therapy.
This article was first published on the Male Psychology Network website in 2018.
Scroll down to join the discussion
Disclaimer: This article is for information purposes only and is not a substitute for therapy, legal advice, or other professional opinion. Never disregard such advice because of this article or anything else you have read from the Centre for Male Psychology. The views expressed here do not necessarily reflect those of, or are endorsed by, The Centre for Male Psychology, and we cannot be held responsible for these views. Read our full disclaimer here.
Like our articles?
Click here to subscribe to our FREE newsletter and be first
to hear about news, events, and publications.
Have you got something to say?
Check out our submissions page to find out how to write for us.
.
Dr Naomi Murphy, currently Clinical Director of the Fens Offender Personality Disorder Pathway Service at HMP Whitemoor, is a Consultant Clinical & Forensic Psychologist with a long-standing interest in the psychological needs of male offenders.